Escherichia coli infection, a negative prognostic factor on the evolution of patients with surgical diseases
DOI:
https://doi.org/10.55779/nsb14311344Keywords:
bacterial infections, Escherichia coli, hemolytic uremic syndrome, multiresistant bacteria resistant to antibiotic therapyAbstract
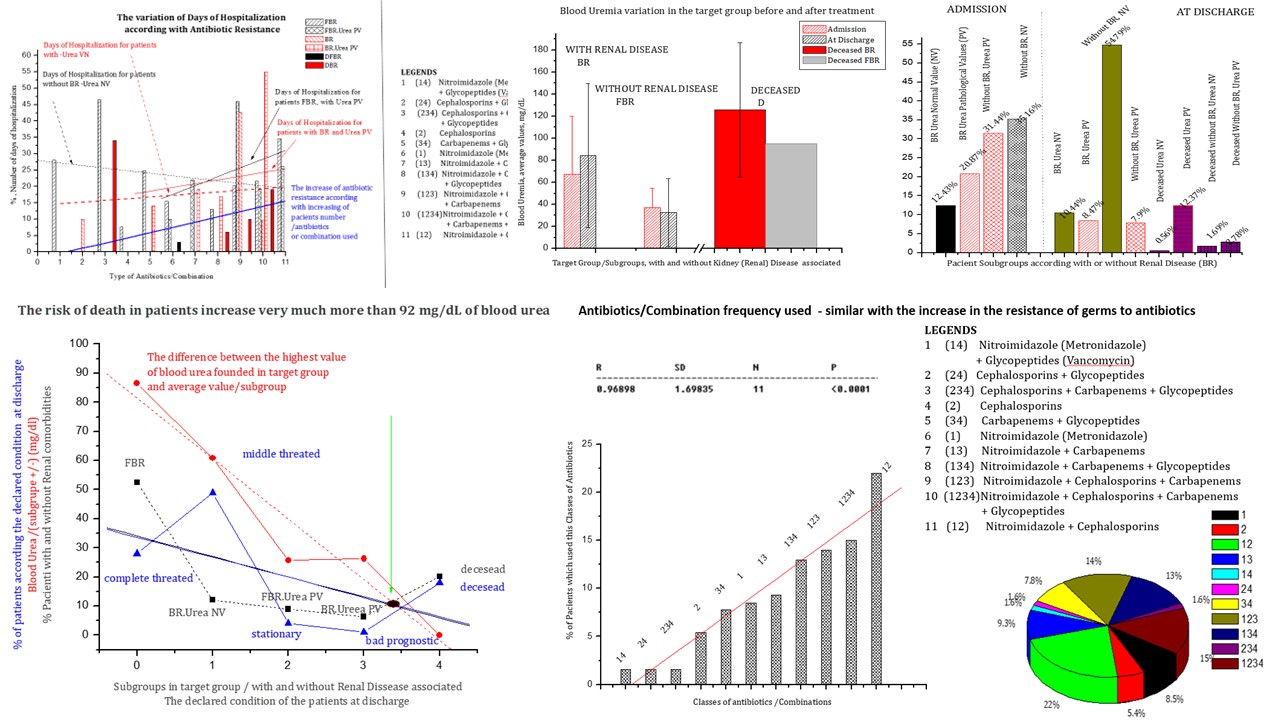
The bacterium Escherichia coli, one of the most studied bacteria in the world, with the greatest epidemiological impact, includes both commensal and pathogenic strains, with a genome that can be extremely varied both in size and genetic content, and it also can produce numerous diseases with specific symptoms. The vast majority of these strains can cause severe gastrointestinal diseases, hemolytic uremic syndrome, hemorrhagic colitis, renal failure and even death. Hemolytic uremic syndrome can be a consequence of the presence of Escherichia coli infection in gastrointestinal diseases. In this study, uremia in patients with and without the declared renal comorbidity, was negatively correlated with the response to antibiotic treatment. The increase of uremia above 92 mg/dl increases the risk of death. The highest risk categories include people with kidney disease like comorbidities starting with admission in surgical and intensive care wards in IRGH Cluj-Napoca, having as main diagnosis of hospitalization surgical digestive diseases. The occurrence of Coli pathogen infection was associated with increased morbidity and mortality rates in patients included in the study. In these patients, it was noticed the need to introduce therapy with increasingly complex antibiotic formulas, which lead to an increase in the duration and cost of hospitalization. In the studied group, due to E coli infection at admission, uremia had an average value of 23.99mg/dl +/-8.987(SD) in the case of patients without kidney disease, the number of patients with normal uremia values was lower than that of those with increased values of uremia. In the case of patients with confirmed kidney disease, uremia had mean values of 65.76 mg/dl +/-52.41(SD). At discharge, both in the case of patients with renal disease and in the case of those without confirmed renal disease, the number of patients with normal values of uremia was higher than those with pathological values, this proportion being reversed in the case of deceased patients where the number of patients with values pathological urea levels were significantly higher than those with normal values, proving kidney damage.
Metrics
References
Ahmed S, Hansen C, Dahlkilde AL, Herrero-Fresno A, Pedersen KS, Nielsen JP, Olsen JE (2021). The effect of colistin treatment on the selection of colistin-resistant Escherichia coli in Weaner pigs. Antibiotics 10:465. https://doi.org/10.3390/antibiotics10040465
Akuzawa N, Kurabayashi M (2018). Native valve endocarditis due to Escherichia coli infection: a case report and review of the literature. BMC Cardiovascular Disorders 18:1-9. https://doi.org/10.1186/s12872-018-0929-7
Alanazi MQ, Alqahtani FY, Aleanizy FS (2018). An evaluation of E. coli in urinary tract infection in emergency department at KAMC in Riyadh, Saudi Arabia: retrospective study. Annals of Clinical Microbiology and Antimicrobials 17:1-7. https://doi.org/10.1186/s12941-018-0255-z
Chinchilla-López P, Cruz-Ramón V, Ramı́rez-Pérez O, Méndez-Sánchez N (2018). Gastroenteritis in an adult female revealing hemolytic uremic syndrome: case report. World Journal of Gastroenterology 24:763. https://doi.org/10.3748/wjg.v24.i6.763
Dhingra S, Rahman NA, Peile E, Rahman M, Sartelli M, Hassali MA, . . . Haque M (2020). Microbial resistance movements: an overview of global public health threats posed by antimicrobial resistance, and how best to counter. Frontiers in Public Health 8:535668. https://doi.org/10.3389/fpubh.2020.535668
Fournier D, Chirouze C, Leroy J, Cholley P, Talon D, Plesiat P, Bertrand X (2013). Alternatives to carbapenems in ESBL-producing Escherichia coli infections. Médecine et Maladies Infectieuses 43:62-66. https://doi.org/10.1016/j.medmal.2013.01.006
Geerlings SE (2008). Urinary tract infections in patients with diabetes mellitus: epidemiology, pathogenesis and treatment. International Journal of Antimicrobial Agents 31:54-57. https://doi.org/10.1016/j.ijantimicag.2007.07.042
Golli AN-L, Nițu FM, Bălășoiu MA, Rascu S, Lungu MA, Dinescu SN, . . . Olteanu M (2019). Microbiological profile and antibiotic resistance pattern of bacterial uropathogens among hospitalized patients. Farmacia 67:167-173.
Harkins VJ, McAllister DA, Reynolds BC (2020). Shiga-toxin E. coli hemolytic uremic syndrome: review of management and long-term outcome. Current Pediatrics Reports 8:16-25. https://doi.org/10.1007/s40124-020-00208-7
Hartadi EB, Effendi MH, Plumeriastuti H, Sofiana ED, Wibisono FM, Hidayatullah AR (2020). A review of enterotoxigenic Escherichia coli infection in piglets: Public health importance. Systematic Reviews in Pharmacy 11:687-698.
Jang J, Hur H-G, Sadowsky MJ, Byappanahalli MN, Yan T, Ishii S (2017). Environmental Escherichia coli: ecology and public health implications—a review. Journal of Applied Microbiology 123:570-581. https://doi.org/10.1111/jam.13468
Jones LF, Meyrick J, Bath J, Dunham O, McNulty CA (2019). Effectiveness of behavioural interventions to reduce urinary tract infections and Escherichia coli bacteraemia for older adults across all care settings: a systematic review. Journal of Hospital Infection 102:200-218. https://doi.org/10.1016/j.jhin.2018.10.013
Karam MR, Habibi M, Bouzarz S (2019). Urinary tract infection: Pathogenicity, antibiotic resistance and development of effective vaccines against uropathogenic Escherichia coli. Molecular Immunology 108:56-67. https://doi.org/10.1016/j.molimm.2019.02.007
Khalid M, Andreoli S (2019). Extrarenal manifestations of the hemolytic uremic syndrome associated with Shiga toxin-producing Escherichia coli (STEC HUS). Pediatric Nephrology 34:2495-2507. https://doi.org/10.1007/s00467-018-4105-1
Kot B (2019). Antibiotic resistance among uropathogenic. Polish Journal of Microbiology 68:403-415.
Laura B, Federica G, Francesca V, Stefano K, Gioacchino L, Gian LDA, Claudio R (2018). Hemolytic uremic syndrome: differential diagnosis with the onset of inflammatory bowel diseases. Acta Bio Medica: Atenei Parmensis 89(Suppl 9):153. https://doi.org/10.23750/abm.v89i9-S.7911
Lee DS, Lee S-J, Choe H-S (2018). Community-acquired urinary tract infection by Escherichia coli in the era of antibiotic resistance. BioMed Research International. https://doi.org/10.1155/2018/7656752
Li J, Rettedal EA, van der Helm E, Ellabaan M, Panagiotou G, Sommer MO (2019). Antibiotic treatment drives the diversification of the human gut resistome. Genomics, Proteomics & Bioinformatics 17:39-51.
Ny S, Edquist P, Dumpis U, Gröndahl-Yli-Hannuksela K, Hermes J, Kling AM, ... Group NU (2019). Antimicrobial resistance of Escherichia coli isolates from outpatient urinary tract infections in women in six European countries including Russia. Journal of Global Antimicrobial Resistance 17:25-34. https://doi.org/10.1016/j.jgar.2018.11.004
Onyenweaku Florence C, Ifeanyi OE, Nwandikor Uzoije U (2018). A review on heamolytic uremic syndrome. International Journal of Current Research in Medical Sciences 4(3):80-92.
Popa GL, Preda M, Gheorghe S-A, Popa M-I (2016). Infectii intestinale ale epocii moderne: diareea calatorului prin ochiul clinicianului/Intestinal infections of the modern era: travelers' diarrhea through the clinician's eye. Infectio 46:5.
Pormohammad A, Nasiri MJ, Azimi T (2019). Prevalence of antibiotic resistance in Escherichia coli strains simultaneously isolated from humans, animals, food, and the environment: a systematic review and meta-analysis. Infection and Drug Resistance 12:1181. https://doi.org/10.2147/IDR.S201324
Pouwels KB, Muller-Pebody B, Smieszek T, Hopkins S, Robotham JV (2019). Selection and co-selection of antibiotic resistances among Escherichia coli by antibiotic use in primary care: an ecological analysis. PLoS One 14:e0218134. https://doi.org/10.1371/journal.pone.0218134
Roth N, Käsbohrer A, Mayrhofer S, Zitz U, Hofacre C, Domig KJ (2019). The application of antibiotics in broiler production and the resulting antibiotic resistance in Escherichia coli: A global overview. Poultry Science 98:1791-1804. https://doi.org/10.3382/ps/pey539
Russotto V, Cortegiani A, Fasciana T, Iozzo P, Raineri SM, Gregoretti C, . . . Giarratano A (2017). What healthcare workers should know about environmental bacterial contamination in the intensive care unit. BioMed Research International. https://doi.org/10.1155/2017/6905450
Talan DA, Takhar SS, Krishnadasan A, Abrahamian FM, Mower WR, Moran GJ, . . . EMERGEncy ID Net Study Group (2016). Fluoroquinolone-resistant and extended-spectrum β-lactamase–producing Escherichia coli infections in patients with pyelonephritis, United States. Emerging Infectious Diseases 22:1594. https://doi.org/10.3201/eid2209.160148
Tarr GA, Downey E, Pang X-L, Zhuo R, Strickland AJ, Ali S, . . . Freedman SB (2022). Clinical profiles of childhood astrovirus-, sapovirus-, and norovirus-associated acute gastroenteritis in pediatric emergency departments in Alberta, 2014–2018. The Journal of Infectious Diseases 225:723-732. https://doi.org/10.1093/infdis/jiab429
Tenney J, Hudson N, Alnifaidy H, Li JT, Fung KH (2018). Risk factors for aquiring multidrug-resistant organisms in urinary tract infections: a systematic literature review. Saudi Pharmaceutical Journal 26:678-684. https://doi.org/10.1016/j.jsps.2018.02.023
Travert B, Dossier A, Jamme M, Cointe A, Delmas Y, Malot S, ... des Microangiopathies Thrombotiques CDR (2021). Shiga toxin–associated hemolytic uremic syndrome in adults, France, 2009–2017. Emerging Infectious Diseases 27(7):1876. https://doi.org/10.3201/eid2707.204638
Valilis E, Ramsey A, Sidiq S, DuPont HL (2018). Non-O157 Shiga toxin-producing Escherichia coli—A poorly appreciated enteric pathogen: Systematic review. International Journal of Infectious Diseases 76:82-87. https://doi.org/10.1016/j.ijid.2018.09.002
van Driel AA, Notermans DW, Meima A, Mulder M, Donker GA, Stobberingh EE, Verbon A (2019). Antibiotic resistance of Escherichia coli isolated from uncomplicated UTI in general practice patients over a 10-year period. European Journal of Clinical Microbiology & Infectious Diseases 38:2151-2158. https://doi.org/10.1007/s10096-019-03655-3
Wassenaar TM (2016). Insights from 100 years of research with probiotic E. coli. European Journal of Microbiology and Immunology 6:147-161. https://doi.org/10.1556/1886.2016.00029
Zhen X, Lundborg CS, Sun X, Hu X, Dong H (2019). Economic burden of antibiotic resistance in ESKAPE organisms: a systematic review. Antimicrobial Resistance & Infection Control 8:1-23. https://doi.org/10.1186/s13756-019-0590-7
Downloads
Published
How to Cite
Issue
Section
License
Papers published in Notulae Scientia Biologicae are Open-Access, distributed under the terms and conditions of the Creative Commons Attribution License.
© Articles by the authors; licensee SMTCT, Cluj-Napoca, Romania. The journal allows the author(s) to hold the copyright/to retain publishing rights without restriction.
License:
Open Access Journal - the journal offers free, immediate, and unrestricted access to peer-reviewed research and scholarly work, due SMTCT supports to increase the visibility, accessibility and reputation of the researchers, regardless of geography and their budgets. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles, or use them for any other lawful purpose, without asking prior permission from the publisher or the author.













.png)